Case study presentation by Dr Melanie Salmon TRE Trainer, Somerset West, Western Cape, South Africa, June 2016
I would like to thank Kirsty Gorfil, Caren Gorfil and Don Jones, for the generous and full permission to allow me to tell this remarkable and inspiring story.
Introduction
I met Caren Gorfil in Johannesburg on 28th February 2016. We were both attending a family wedding. I noticed that she was distracted and on the phone much of the time. My brother mentioned that Caren was supporting her daughter Kirsty who was going through another of her medical crises. He mentioned in passing that Kirsty was Bipolar and had “unusual shaking” during her “attacks”.
My interest was piqued and I offered to talk to Caren if she was interested, as my work involves “shaking”. We planned to meet up the next day. I could see that Caren was stressed and anxious, while maintaining control over her emotions. I decided to be thorough and explore the story fully from the beginning. This is what she told me:
Presenting problem
Caren and Kirsty live in a beautiful residential estate in Umhlanga KZN. Kirsty, now aged 23, had been diagnosed over 3 years ago by a prominent Durban psychiatrist with a very rare form of bipolar that manifested physically. Her symptoms included intermittent severe anxiety &
depression, and generalised pain syndrome. She is on a range of treatment for bipolar including an SSRI antidepressant Cymgen, an anti convulsants, Lamictin & Urbanol for anxiety. This cocktail did not work entirely & she continued to have intermittent violent shaking attacks of mostly her right
arm and right leg, lasting on average an hour or more. These attacks were uncontrollable & were accompanied by extreme pain& followed by exhaustion & migraines. Kirsty also recently went through a course of 30 treatments on a Brainsway machine (deep trans-cranial magnetic stimulation TMS, for treatment of major depressive disorder). The attacks continued even after the
TMS treatment leaving both Kirsty & Caren bewildered & helpless.
History of presenting problem
Birth: 2 months premature, in Special Care baby Unit for 2 weeks on life support
Toddler:
a. Suffered a dislocated right shoulder from dad swinging her. Had to have it attended to in casualty
b. Fell downstairs in a walking ring, landing on her head
Age 7-12: Parents went through an acrimonious divorce.
Age 16 : She developed severe pain down the right arm. She was operated on for a diagnosis of Thoracic Outlet Obstruction Syndrome, to remove a rib on the right side of her neck. While in intensive care post-operatively, she almost died when her lung filled up with fluid because the intercostal drain had been inadvertently clamped off. Luckily her mum was present when Kirsty
became short of breath and went blue and so raised the alarm.
Age 16: After the operation, the right arm pain continued unabated and second operation, a Sympathectomy on the right side of the neck, was performed by a Professor of surgery, to cut the nerves to the right arm. She was pain free for 5 months.
Age 16, “seizures” began: the arm pain escalated and after another month Kirsty had her first “seizure”…twitching starting in the right arm/hand and then full shaking of the right arm and head shaking to the side. Often the shaking spread to the right leg and rest of the body. These attacks were uncontrolled, lasting over an hour, leaving her exhausted and asleep for hours. Admitted to Milpark Hospital for 2 weeks under a neurologist where she was investigated fully and on 24 hours video monitoring. She was witnessed as having 3-4 “seizures per day”… she was always conscious during these . A diagnosis was made of PRIMARY DYSTONIA with DYSTONIC STORMS.
Age 17: Given pharmaceutical treatment for DYSTONIA : Reserpine, Rivotril, Lioresal, Akineton,Sinemet, Celebrex and Cymbalta. None worked as the right arm pain and “fits” continue unabated. Brain surgery was discussed, DBS.
DYSTONIA Medical Research Foundation What is Deep Brain Stimulation?
Deep brain stimulation (DBS) is a surgical procedure used to treat a variety of neurological disorders,including movement dystonia. A battery-powered stimulator —essentially a brain pacemaker—is surgically implanted and delivers electrical stimulation to the areas of the brain associated with dystonia. The procedure is completed in several phases: pre-surgical assessment and work-up, implanting the leads, implanting the stimulator, activating the stimulator, and programming the stimulation settings. Adult patientsare typically awake during the process of implanting the leads and participate in the placement by responding to questions and instructions from the surgical team. It can take weeks or months for individuals
to achieve full benefit.
Age 17: Mum refused a brain implant for Kirsty and instead agreed to seek an expert opinion in the USA. They attended 2 units specialisting in “movement disorders”, one in New York and the Emory Clinic in Atlanta. The specialists there were dismissive of the diagnosis of Dystonia and told Kirsty to come off all meds; symptoms continue as before. They suggested she saw a psychiatrist and were unable to explain the shaking fits.
Age 18: admitted to the Epilepsy Unit, Durban for full monitoring and work up- results showed conclusively that Kirsty did not have any form of Epilepsy…EEG etc all normal during “fits”.
Age 18: Kirsty was sent to a psychiatrist who diagnoses “Conversion Disorder”. This is a form of somatisation according to the DSM IV, a physical manifestation of psychological problems. Kirsty was put on further psychiatric meds to depress her nervous system.
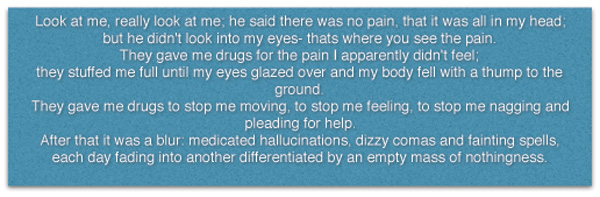
Kirsty had missed most of her last year of school. She attended drama class and did a short written project about her experience, part of which she has agreed for me to share here:
 Age 23, 2015: Finally, with Kirsty’s symptoms unrelieved, a second Psychiatric opinion was sought with a Psychiatrist in Durban. This is when the final agreed diagnosis of
Age 23, 2015: Finally, with Kirsty’s symptoms unrelieved, a second Psychiatric opinion was sought with a Psychiatrist in Durban. This is when the final agreed diagnosis of
“A very rare form of Bipolar, manifesting in physical disorders rather than mood disorders”,
was made and the treatment above, prescribed.Sadly these drug combinations are also not working. Kirsty is largely house bound, unable to drive and is worried about being labelled a “freak”.
My opinion before meeting Kirsty
Having heard this detailed account: I wondered if Bipolar may be a mis-diagnosis and that Kirsty could be having normal tremor release from the trauma of several surgeries to the right arm and neck. The original trauma was a dislocated right shoulder at three years of age. There is certainly enough stress and trauma in her history to suggest that her autonomic nervous system is in a dysregulated state of fight and flight, spontaneously releasing adrenalin and cortisol through natural tremors. Once explained to Caren, I was invited me to come to her home to work with Kirsty on 9 March, should Kirsty agree to it.
First Meeting with Kirsty Gorfil 9 March, in Durban
I flew to Durban to stay with Caren for 2 days. I met Kirsty the night before we were scheduled to do TRE, and used the time to explore her hopes and fears. She was understandably skeptical and withdrawn and reluctant to try yet another treatment. She asked why my method should help when everything else had failed. I explained to her the physiology of trauma and how the autonomic nervous system, over time, becomes dysregulated when trauma is chronic or severe. The fluctuation between fight and flight sympathetic over-drive and the vagal freeze response, were probably producing her “bipolar” symptoms as well as the tremors in the areas affected by surgical trauma. I explained that what I had to offer with TRE was non-invasive and just might help. She agreed to do TRE the following day with me but I could see she was very doubtful that anything would help. I understood why she was not willing to trust me.
I asked her what she would like to get from doing TRE and she said simply
“ I want my life back”
First TRE session 10 March am
During the exercises, I noticed that Kirsty’s right hand and arm were shaking uncontrollably. She looked miserable and low in energy.
First tremor went well: When the tremors activated in the hip abductors, hip flexors and pelvis the arm tremors stopped; She tremored only in the lower body region. I allowed her to tremor for 45 minutes. She self-regulated 3 x successfully and was encouraged to discover that she had full control over her tremors.
Integration time: 2 hours deep sleep
Afterwards: Kirsty, smiling, said she felt more relaxed than she had felt in years
Second Session 10 March pm
Again Kirsty tremored in the lower half, regular equal tremors without any emotional discharge. At no time did she flood or dissociate. She was happily present to her experience and asked questions to understand the process. In particular her spontaneous arm shaking went away completely and did not return again at any time.
Tremor time : 45 minutes; integration time 1.5 hours
Third and fourth sessions together with Mum 11 March am
I invited Caren to join us for TRE and I facilitated both of them over a one hour session. Both had good, sustained release without any flooding or dissociation. Karen was also much more relaxed and at ease after her tremor sessions. Kirsty felt supported by having her Mum join her and I gave them permission to include Kirsty’s boyfriend Don in future sessions.
TRE plan going forwards
Having discussed the TRE journey at length, we agreed that Kirsty would continue with regular TRE, supported by her mum and boyfriend. They would do TRE 3-4 times a week, for an average of 20-30 minutes each time. I gave them access to me for any questions or untoward symptoms that may arise after I left. We planned a review visit at my home in Somerset West in 5 weeks time. When I left I was aware at the significant level of groundedness achieved by both Kirsty and her Mum in the space of 4 tremors over 2 days. I felt confident that we were on the right track, in destressing the nervous system through the natural discharge of stress through psoas tremoring. I made sure that Kirsty would stay on her medications for the time being.
Follow-up visit to Somerset West 13 April 2016 (5 weeks of TRE)
I noticed a remarkable change in both Kirsty and her mum. They were relaxed and grounded and seemed to be very light, happy, smiling and grateful for this journey. Caren told me that the changes in Kirsty are remarkable and feels she is her old self again. Kirsty says she has her life back again. Almost all original symptoms are gone( back pain, depression, migraine etc).
Tremor history:
Both have kept up tremoring 3-4 x weekly for approximately 20-30 minutes. There have been no unmanageable discharges during or after TRE and emotional states such as irritation or sadness were “bearable”.
I facilitated each of them alone and together over the two days with me. Both of them have tremors located in the lower half of the body. Kirsty tells me that she does not get spontaneous tremors in the right arm any longer. She is also attuned to her body’s need for release and if she misses TRE her body lets her know. She is enjoying this positive relationship with her organismic needs and feels fully in control.
Follow-up visit 24 June 2016, Durban (3 months of TRE)
I had received positive emails and phone messages during our time away from each other, that Kirsty remained well and improving every week. I was not prepared for the huge changes I saw in her when I returned to Durban on 23rd June. She was warm, smiling, laughing openly and easily… she gave me a huge hug which expressed her gratitude. I found myself looking at a normal, optimistic and confidant young women whose future was opening up in front of her. No longer was there the withdrawn, averted gaze, the doubtful expression, the extreme anxiety… but a different zest for living. Kirsty had indeed got her life back!
I interviewed Kirsty and Don:
Melanie: What are the benefits to you of TRE over these past 3 months ?
Kirsty: Its changed something so negative in my life into something thats so positive. I never had control over the shaking which were called “attacks”, It was scary, nothing I could control…now I have control back, that its a positive thing, my body healing itself… I have more light in my life… its enabled me to feel positive about moving forward.
Melanie: How are the symptoms you had before TRE : depression, back pain, headaches and so on?
Kirsty: Not 100% gone, due to the fact thats Im still on so much medication… which my body no longer needs… I dont think EVER needed… and trying to get off that medication is really tough…those side-effects are not completely disappeared yet. I am being weaned off my medication now, since 3 weeks ago and I am already feeling lighter and healthier
Melanie: What was it like to see your Psychiatrist again? I mean he diagnosed you with Bipolar.
Kirsty: It was very strange… even as I walked in he said “you’re doing well, aren’t you!” He could immediately see a difference in me….that I was better… it was daunting trying to explain to him why I am better, because he’s a doctor…I talked about you, coming from the medical field, that helped a bit…
and then I offered to show him… I went into the bridge position for 2 minutes and then tremored for 2 minutes….he seemed astounded… very interested, very curious…he satisfied himself that this was what I was having before, yet here I was in control and obviously very peaceful….I think that was quite a shock for him to see… and his words, not mine were: “your illness is now a cure”……and he’s very happy now to reduce my medication until I am off all drugs.
Melanie: So getting back-up like this from your mainstream Doctor must be very encouraging?
Kirsty: Yes he is happy… I know its a process but the fact is I am going to be medication free as well as being free of my illness!…. I always fought against people telling me I was sick, that there was something wrong with me…I had been diagnosed so many times with Bipolar, but I was never at peace with it, I always fought against it…people told me its going to be so much easier when I accept it, that its going to be OK… a lot of people deal with Bipolar, its not some strange thing, its very common….so normal… but NO… this is not right, its not me, I am not sick! so now, not to have that label across my forehead is incredibly freeing…it opens up so many possibilities…before I had a road-block on every single road I was trying to get down… and now I dont!
Melanie, to Don: Don, I can see that you are enjoying doing TRE with Kirsty. Can you share what its been like to be with Kirsty during this time?
Don: When Kirsty had her “attacks” so to speak, it was a hard thing to watch… her whole body locking up…no control whatsoever…..you just have to wait it out….since Kirsty has started doing TRE she hasn’t had one “attack”!!……..and I see that she’s a lot more lively…. and happy! Its been
a good process.
Final TRE session Kirsty and Don 24 June Durban
Both Don and Kirsty are having regular, well modulated tremors of mostly the bottom half of the body. There are subtle signs that tremors may be moving up soon, by way of occasional head movement and some finger movement. I facilitated the session with an intervention each and reassured them that with time, tremors may well move to other places when ready to do so. They were grounded and present throughout. Kirsty still needed a long integration time of 1 hour, while Don only had 10 minutes.
Moving forwards
I suggested that they both continue the regularity of TRE at 3-4 x weekly especially while Kirsty is coming off her medications. They have access to me by email and phone but no further follow-up visit is planned.
Comment from Dr Melanie Salmon
I have presented this case study several times to TRE Provider audiences and the overwhelming request was for me to publish my findings on this website. By reaching a wider audience this story may open doors of enquiry and possibility for others.
I personally decided to work with Kirsty myself based on the following :
- Several traumatic medical interventions all pointed back to an original trauma in childhood. They did in turn enhance the trauma. I was curious to explore for myself, if her spontaneous tremoring located in the area of surgery, was a normal organic release of trauma. I was astounded that the trauma history had been missed and that “experts” in “movement disorders” were unaware of normal self-induced body tremors ie neurogenic tremors.
- I am aware that depression and Bipolar disorder are increasing exponentially. I also see how many have had serious traumatic histories. It is recognised in psychiatric circles that the diagnosis and differentiation between PTSD, ADHD and BIPOLAR is often difficult and that they share common symptoms and morbidity and frequently overlap. And yet definitive diagnoses are made and patients put on life long psychiatric drugs to control symptoms. I wonder how often Bipolar may be a mis-diagnosis?
- Hitherto I have turned down requests to use TRE with clients diagnosed with BIPOLAR, especially if they are under psychiatric care, are on meds and may be unstable. This is one of the cautions/contra-indications for doing TRE. I therefore was going against what I believed to be sensible practice in doing TRE with Kirsty who had a psychiatric diagnosis. I covered myself by doing TRE 4 x over 2 days and evaluating the response while staying with her all the time. I also had support of the family, who would alert me to any destabilising of Kirsty’s emotional condition. In fact Kirsty showed a very positive grounding response to TRE from the beginning.
In conclusion, I personally will be open to using TRE with clients who come to me with a diagnosis of Bipolar disorder. I will be very careful to take a thorough history to establish trauma, especially from childhood which could lead to dysregulation of the Autonomic Nervous system, with its bipolar features of fluctuation between sympathetic over drive and parasympathetic freeze response.
I will provide close evaluation and support throughout and monitor that the client is indeed improving while doing TRE regularly. I will encourage the client to work with their Psychiatric specialist and am willing to do so myself if this is feasible.
—————————————-
For more information on trauma and the ANS see
The Brain in Trauma and PTSD with Robert Scaer MD – download pdf below






